Global collaborative care model market is estimated to be valued at USD 1.97 Bn in 2025 and is expected to reach USD 5.46 Bn by 2032, exhibiting a compound annual growth rate (CAGR) of 15.7% from 2025 to 2032. The model aims to enhance patient care by facilitating effective communication and movement of relevant information among a care team. This integrated team usually comprises primary care physicians, care managers, psychiatrists, therapists, and consultants.
Discover market dynamics shaping the industry: Download Free Sample
Increasing prevalence of chronic medical and behavioral health conditions boosts adoption of collaborative care models. Improving reimbursement landscape and emphasis on value-based care are incentivizing healthcare providers and organizations to implement collaborative care programs. The model's proven clinical effectiveness and ability to lower costs boosts its uptake.
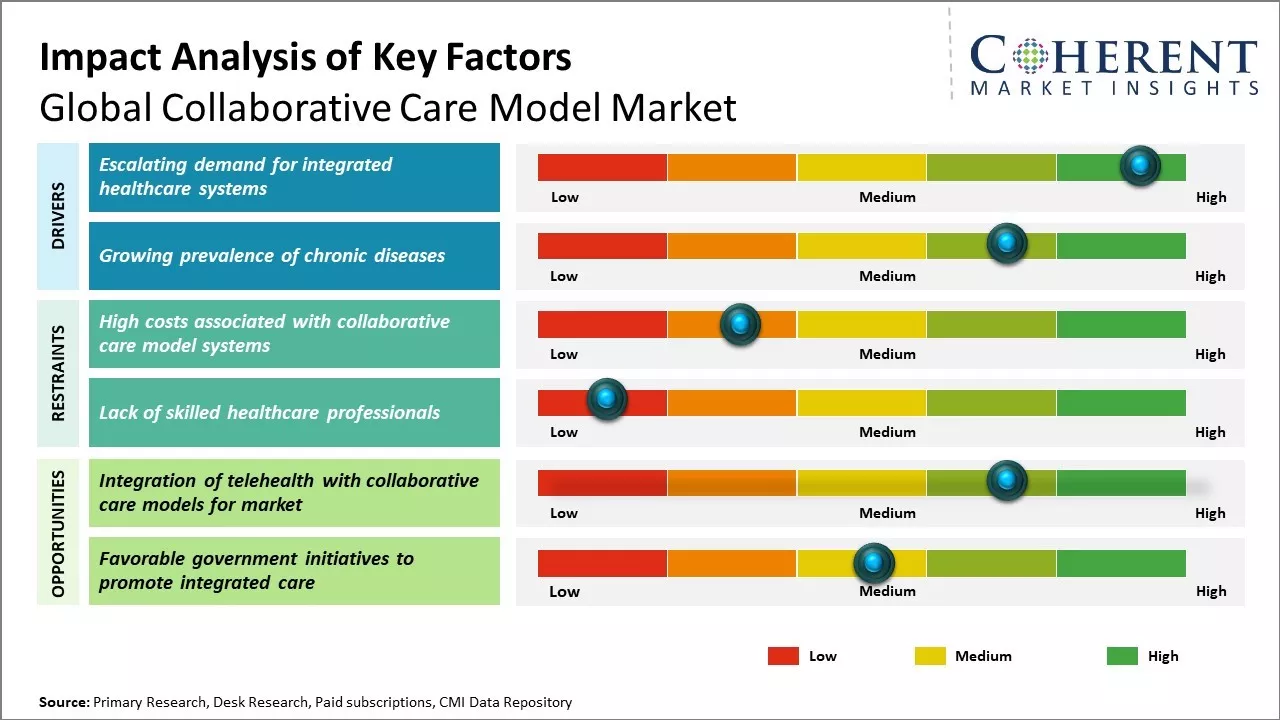
Escalating demand for integrated healthcare systems
Healthcare systems are witnessing increasing pressure in the form of rising costs of treatment and limited resources. There has been growing need to cut costs and enhance efficiency of service delivery mechanism. This has boosted demand for collaborative care models where different healthcare service providers work in a coordinated manner to offer seamless healthcare services. Siloed approach of the past where individual departments such as primary care, specialty care, hospitals, and others worked independently is no longer relevant in the current scenario. Patients need all aspects of care to be well aligned right from preventive services, diagnostics, treatment, rehabilitation and others. Disjointed care often results in duplication of services, gaps in care continuum and higher costs. This highlights the requirement of collaborative networks where all stakeholders co-create strategic partnerships and information is shared seamlessly across care settings through digital platforms. With healthcare becoming increasingly complex due to advancement in treatment options, patients have complex needs. Their conditions often cut across multiple departments and resource pools. Coordinated care helps facilitate comprehensive management of health issues. It ensures proper communication flow between different providers and keeps patient needs and preferences at the focus of care delivery. This assures a more joined-up approach towards achieving optimal health outcomes.
Get actionable strategies to beat competition: Download Free Sample
Growing prevalence of chronic diseases
Non-communicable diseases have emerged as a leading cause of mortality and morbidity across both developed and developing world. Countries like U.S., China and India faces a heavy disease burden of chronic illnesses such as diabetes, cancer, cardiovascular conditions and respiratory disorders. As per estimates, over 60% of global fatalities are due to chronic conditions currently. This poses huge economic implications in terms of medical expenditures, loss of productivity and quality of life. Chronic diseases frequently require long term treatment, management, monitoring and lifestyle modifications. A single physician may not be able to satisfactorily address all aspects especially when co-morbidities exist. Patients find it difficult to navigate the complex care processes which span multiple care settings, specialties and service lines. Lack of coordination raises risks of suboptimal care, hospital re-admissions, medical errors and duplications. It also affect patients' adherence to treatment plans in the absence of streamlined guidance and support structures. Collaborative care models help foster integrated, patient-centric approaches for chronic illness care. Empanelment of multi-disciplinary care teams allows comprehensive oversight over patients' conditions. Co-located services in community-based facilities facilitate convenient access. Shared care plans and interoperable health records exchange timely updates while keeping patient preferences and goals at heart. This helps enhance quality of life as well as clinical outcomes for patients living with chronic diseases.
Key Takeaways from Analyst:
Global collaborative care model market growth is driven by rising demand for integrated healthcare services globally, growth in elderly population worldwide, and increased acceptance of collaborative care approaches. Rising prevalence of chronic diseases is can also boost demand for improved collaborative care models across various countries.
High costs of implementing collaborative care programs and lack of reimbursements policies for collaborative services can hamper the market growth. Lack of skilled professionals can pose challenges for seamless execution of collaborative care approaches particularly across price-sensitive developing nations.
North America region currently dominates the l market, owing to factors like favorable reimbursement structures, adoption of digital health approaches, and presence of major players in countries like the U.S. and Canada. Asia Pacific is likely to witness the fastest growth over the forecast period due to rapid economic development, growing medical tourism, and rising focus on multidisciplinary team-based care in countries like China, India and Japan.
Collaborative care model industry appears set for upbeat expansion due to continuous support from organizations like WHO promoting integrated healthcare models globally. Increased focus on patient-centered approaches also works in favor of collaborative care market players worldwide. Widespread deployment of digital collaboration platforms offers lucrative opportunities for players.
Market Challenges: High costs associated with collaborative care model systems
Global collaborative care model market growth can be hampered by high costs associated with implementation and management of collaborative care model systems. Developing the necessary infrastructure for proper coordination between different healthcare providers, continuous monitoring of patients, and effective communication requires substantial investment. Organizations need to invest in technologies like electronic health records, patient portals, care coordination software and telehealth solutions to facilitate collaborative care. These must also hire additional staff like care managers, behavioral health specialists and social workers to effectively support the collaborative care model. All these factors contribute to high operating costs. The upfront capital required and ongoing expenses of managing these systems can pose significant financial burdens, particularly for smaller healthcare providers. The return on investment also takes a long time, making it difficult to prove the value in the short term. This acts as a barrier for many organizations to adopt collaborative care models.
Market Opportunities: Integration of telehealth with collaborative care models for market
Integration of telehealth with existing collaborative care models can offer market growth opportunities. The COVID-19 pandemic has boosted demand and acceptance of telehealth solutions globally. Leveraging digital technologies allows collaborative care teams to monitor and coordinate care for patients remotely using virtual visits. This helps address some of the challenges around high travel costs for home visits or frequent in-person meetings between different providers. Telehealth also improves access and reach and makes collaborative care more convenient for patients living in remote locations. When combined with collaborative care models, telehealth can play a key role in enhancing care coordination, managing chronic conditions more effectively and reducing healthcare costs in the long run. Rising patient comfort with virtual care options can lead to acceptance and popularity of technology-enabled collaborative care models.
Discover high revenue pocket segments and roadmap to it: Download Free Sample
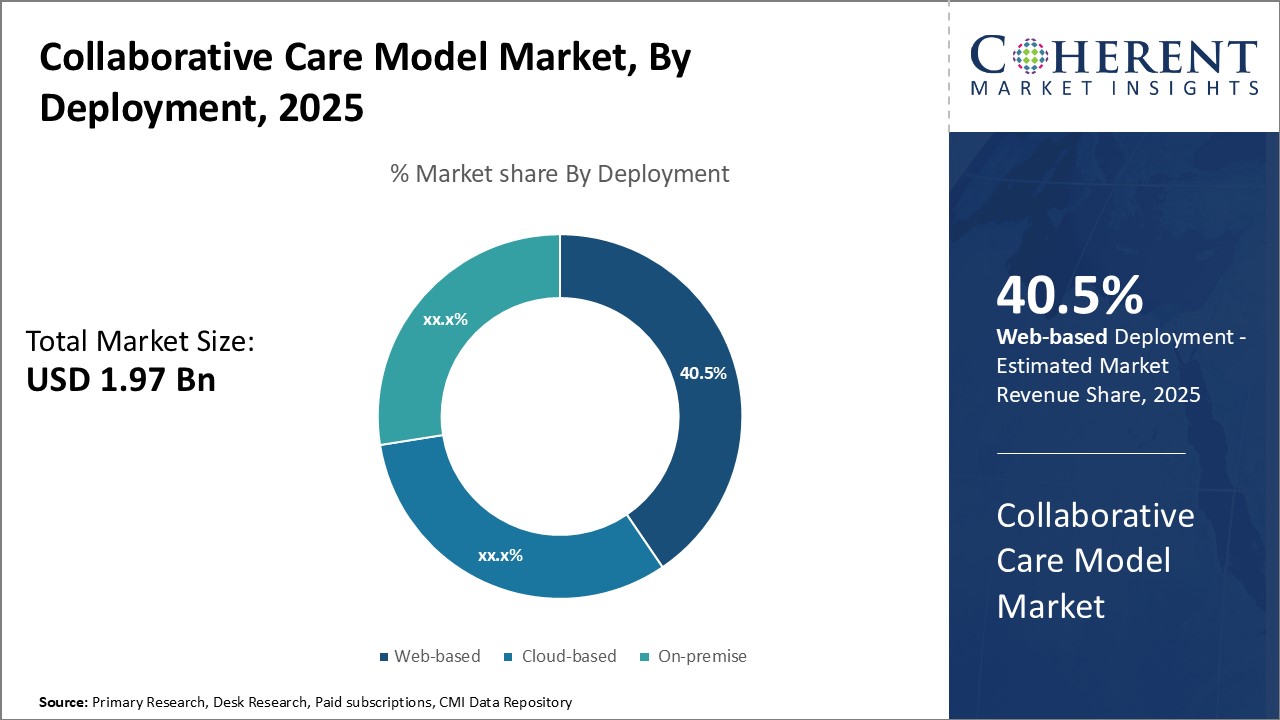
By Deployment- Convenience and Cost-Effectiveness Boosts Demand for Web-based Deployment
In terms of deployment, web-based segment is estimated to contribute the highest market share of 40.5% in 2025 due to its convenience and cost-effectiveness. Web-based collaborative care model requires minimal infrastructure and upfront investment. Healthcare organizations, particularly smaller practices and clinics, find the zero-infrastructure requirement and subscription-based pricing of web-based solutions highly appealing. These do not need to spend on hardware, servers, or related IT resources as these are hosted on remote cloud infrastructure. Maintenance and upgrades are also handled by the solution provider, thus, eliminating the need for in-house technical support. This plug-and-play nature makes web-based collaborative care models very easy to set up and manage. These can be accessed from anywhere through an internet connection, allowing seamless collaboration between dispersed care teams. The pay-as-you-go pricing of most offerings also helps organizations to control costs and eliminate large upfront payments.
By Application- Focus on Population Health Drives Popularity of Population-based Care
In terms of application, population-based care segment is estimated to contribute the highest market share of 42.5% in 2025 due to growing industry focus on preventive care, risk stratification, and overall population health management. Population-based collaborative care applications are specifically designed to organize patient data according to geographic boundaries or demographic characteristics. These help healthcare providers to gain a comprehensive view of community health risks, disease burdens, and social determinants. This allows deployment of proactive intervention programs targeting at-risk demography. These could include disease management registries, preventive screening reminders, remote patient monitoring solutions, lifestyle management programs, and others. Such population health-centric approaches are clinically proven to reduce overall burden on healthcare systems through early detection and prevention of illnesses.
By End User- Prevalence of Chronic Diseases Boosts Adoption in Hospitals and Clinics
In terms of end user, hospitals and clinics segment is estimated to contribute the highest market with 45.5% in 2025 share of, due to high burden of complex, chronic diseases treated at hospitals. Long-term conditions such as cancer, diabetes, heart disease require multifaceted treatment plans spanning various specialties - medical, radiological, dietary, rehabilitation. Coordinating care amongst varied teams and ensuring compliance becomes challenging. Collaborative care models streamline communication between departments, consolidate patient history, and facilitate collaborative decision making. These also enable long-distance consultation and oversight critical for effective chronic disease management. As hospitals endeavor to enhance healthcare quality and reduce readmission rates, these are increasingly adopting such collaboration platforms. Furthermore, a large patient inflow through hospitals necessitates optimized care coordination to improve staff efficiency and cut turnaround times.
Need a Different Region or Segment? Download Free Sample
North America region currently dominates the global collaborative care model market, with an estimated market share of 41.8% in 2025. . This can be attributed to the widespread adoption of value-based care and emphasis on population health management approaches within the region. Integrated and collaborative care models are seen as effective ways to improve outcomes and reduce costs. Several large provider networks and Accountable Care Organizations in the U.S. have invested heavily in technologies, care coordination programs, and workforce training centered around collaborative care. The presence of leading solution vendors and consultants has also enabled swift implementation of collaborative programs across care settings. With established frameworks for data sharing and interoperability, collaborative initiatives have found strong support within the North American healthcare ecosystem.
Asia Pacific is poised to be the fastest growing regional market for collaborative care model. Rapid rise in chronic diseases and increasing focus on multidisciplinary care boosts adoption. Countries like China, India, Japan, and South Korea are witnessing significant growth in hospital partnerships, community health programs, and digital health solutions that employ collaborative approaches. As the population ages and seeks higher quality outcomes, collaborative care is gaining prominence as an effective care model for integrated healthcare delivery. While still early in the adoption curve compared to mature Western markets, APAC countries are expected to ramp up investments aggressively to capitalize on collaborative solutions and consultancy offerings.
Collaborative Care Model Market Report Coverage
| Report Coverage | Details | ||
|---|---|---|---|
| Base Year: | 2024 | Market Size in 2025: | USD 1.97 Bn |
| Historical Data for: | 2020 To 2024 | Forecast Period: | 2025 To 2032 |
| Forecast Period 2025 to 2032 CAGR: | 15.7% | 2032 Value Projection: | USD 5.46 Bn |
| Geographies covered: |
|
||
| Segments covered: |
|
||
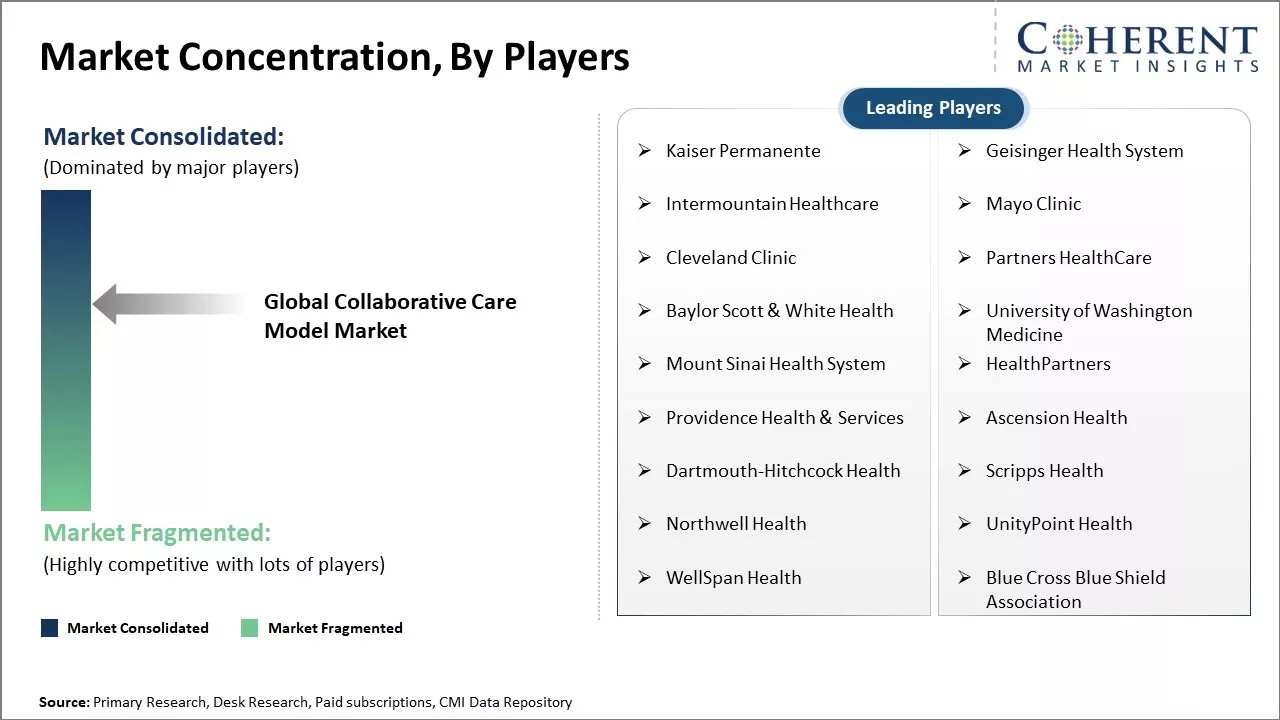
| Companies covered: |
Kaiser Permanente, Geisinger Health System, Intermountain Healthcare, Mayo Clinic, Cleveland Clinic, Partners HealthCare, Baylor Scott & White Health, University of Washington Medicine, Mount Sinai Health System, HealthPartners, Providence Health & Services, Ascension Health, Dartmouth-Hitchcock Health, Scripps Health, Northwell Health, UnityPoint Health, WellSpan Health, Blue Cross Blue Shield Association |
||
| Growth Drivers: |
|
||
| Restraints & Challenges: |
|
||
Uncover macros and micros vetted on 75+ parameters: Get instant access to report
*Definition: Global Collaborative Care Model Market involves offering integrated healthcare delivery services through a collaborative approach between medical providers, behavioral health professionals, and social services organizations. This model promotes coordination and communication between all parties to provide comprehensive care for patients that addresses their medical, behavioral, social, and other determinants of health. Collaborative care aims to improve health outcomes through a team-based approach and accountability across different treatment disciplines involved in patient care.
Share
Share
About Author
Ghanshyam Shrivastava - With over 20 years of experience in the management consulting and research, Ghanshyam Shrivastava serves as a Principal Consultant, bringing extensive expertise in biologics and biosimilars. His primary expertise lies in areas such as market entry and expansion strategy, competitive intelligence, and strategic transformation across diversified portfolio of various drugs used for different therapeutic category and APIs. He excels at identifying key challenges faced by clients and providing robust solutions to enhance their strategic decision-making capabilities. His comprehensive understanding of the market ensures valuable contributions to research reports and business decisions.
Ghanshyam is a sought-after speaker at industry conferences and contributes to various publications on pharma industry.
Missing comfort of reading report in your local language? Find your preferred language :
Transform your Strategy with Exclusive Trending Reports :
Frequently Asked Questions
Joining thousands of companies around the world committed to making the Excellent Business Solutions.
View All Our Clients