Healthcare Reimbursement Market Size and Trends
Global healthcare reimbursement market is estimated to be valued at USD 27.18 Bn in 2025 and is expected to reach USD 84.60 Bn by 2032, exhibiting a compound annual growth rate (CAGR) of 17.6% from 2025 to 2032.
Discover market dynamics shaping the industry: Download Free Sample
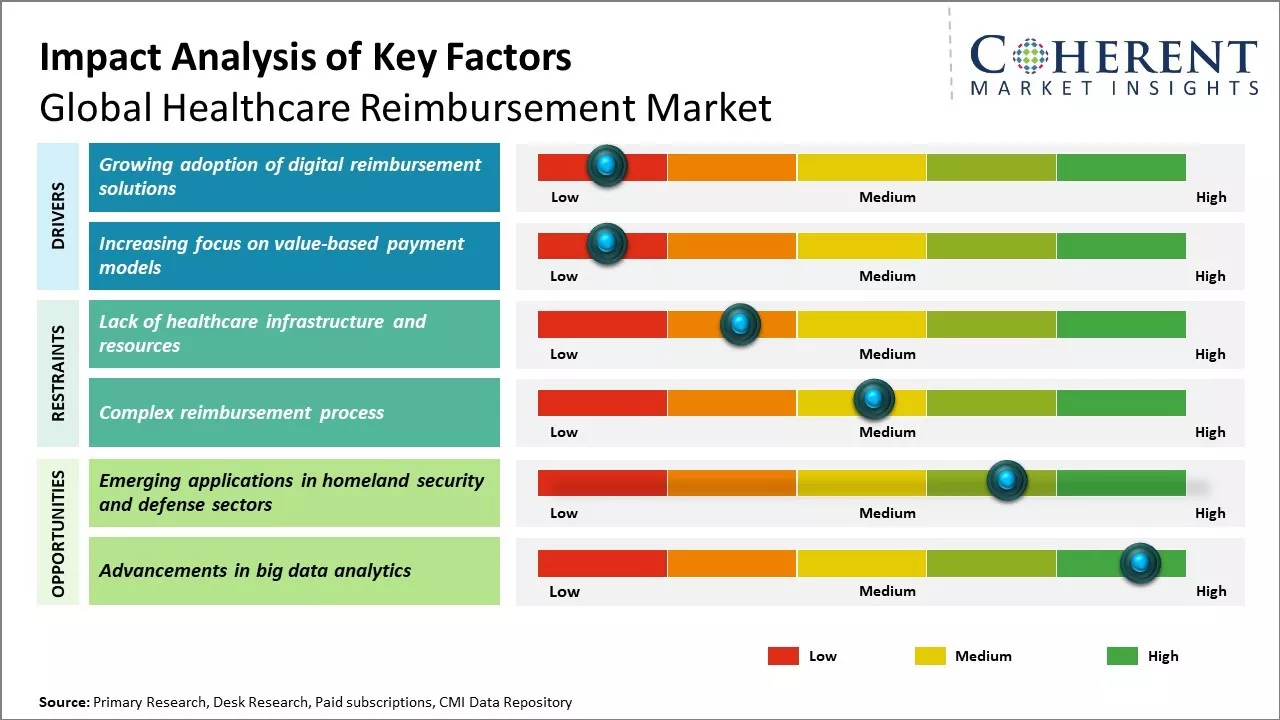
Global healthcare reimbursement market growth is driven by increasing demand for insurance-based medical reimbursement and rising healthcare costs. The introduction of innovative reimbursement models integrating technology and data analytics also drives the market growth. Various governments and regulatory bodies are undertaking several health reforms and initiatives to expand the insurance coverage across countries. Furthermore, increasing geriatric population susceptible to various chronic diseases and rising demand for quality medical care can drive the healthcare reimbursement market growth during the forecast period. However, lack of healthcare resources and infrastructure in developing nations and lack of patient awareness about the reimbursement facilities can hamper the market growth.
Growing adoption of digital reimbursement solutions
With increasing complexities within healthcare systems worldwide, there is growing need to streamline reimbursement processes. Traditional paper-based systems have proven inefficient, thus, leading to higher administrative costs and lengthy wait times for payments. Healthcare providers and insurers are recognizing the value of digital technologies that can automate and optimize reimbursement workflows. Solutions such as cloud-based claims processing platforms allow for real-time status updates, integrated billing and coding functionality, and advanced data analytics capabilities. This helps to address issues like revenue leakage and appeals management. Telehealth and remote patient monitoring have also expanded significantly during the pandemic. As virtual care delivery models become more mainstream, digital platforms will play a critical role in synchronizing reimbursements across care settings. Their ability to integrate with existing clinical and financial systems makes the transition more seamless. As more players in the industry adopt standardized formats like CMS-1500 and UB-04 electronic claim forms, interoperability is improving multi-stakeholder collaboration.
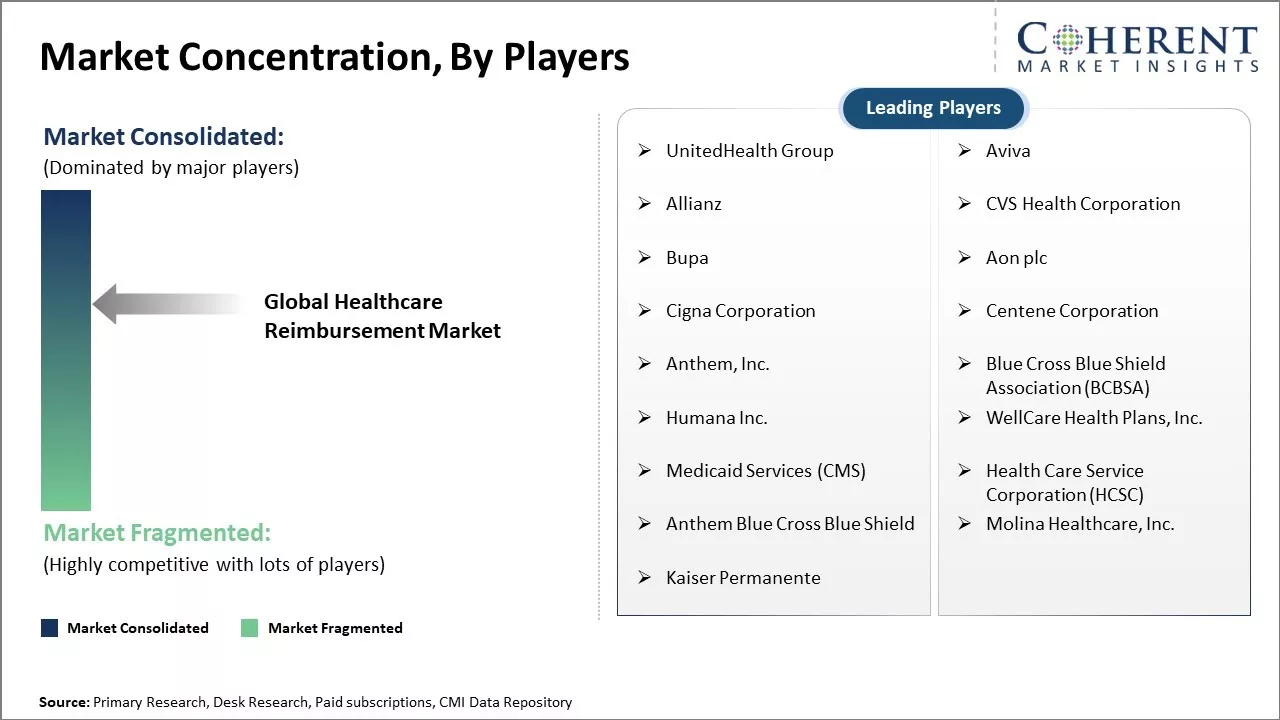
Market Concentration and Competitive Landscape
Get actionable strategies to beat competition: Download Free Sample
Increasing focus on value-based payment models
Traditional fee-for-service models have long dominated healthcare reimbursement. However, rising healthcare costs and the need for better quality and outcomes have led payers and providers to explore alternative payment structures. Value-based models link part of provider reimbursements to quality metrics and performance measures that emphasize preventive care, chronic disease management and patient satisfaction. This shift towards population health encourages collaboration between care settings. Bundled payments and episodic payment models also focus on specific clinical conditions, procedures or episodes of care rather than individual services. These provide financial incentives to improve health outcomes while reducing over-treatment and unnecessary costs. Data analytics plays a key role in evaluating clinical and financial performance across different reimbursement arrangements. Several pilot programs from CMS, private insurers and regional coalitions are already underway to test such models. While challenges remain around complex conditions and small provider networks, the momentum seems poised to make value-based payments a bigger part of healthcare budgets in the coming years. For instance, in April 2024, AHIP, the American Medical Association (AMA), and the National Association of ACOs (NAACOS) released a playbook outlining voluntary best practices to promote the adoption of value-based care in the private sector. This initiative aims to enhance the quality, equity, and affordability of healthcare. The playbook focuses on key areas such as patient attribution methods, financial benchmarks, and effective risk adjustment strategies.
Key Takeaways from Analyst:
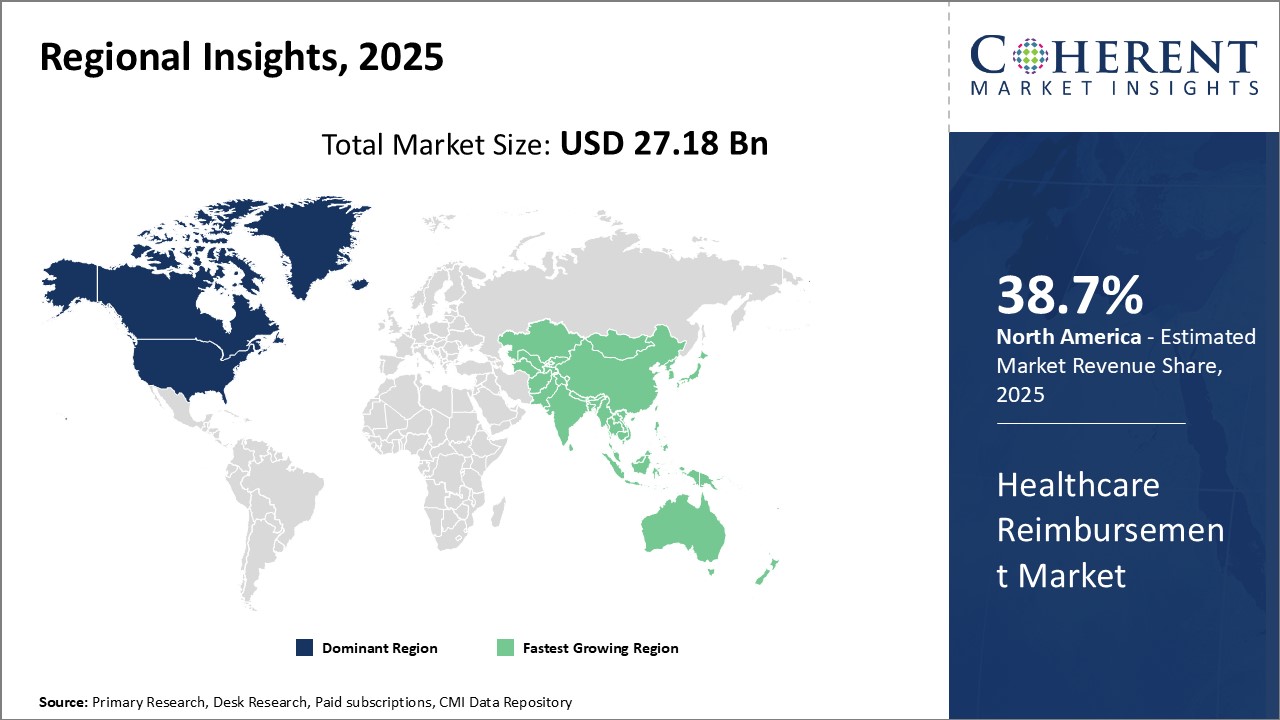
Global healthcare reimbursement market growth is driven by rising healthcare costs as treatments become more expensive. Growing aging population can also drive the market growth as older patients typically require more medical care and services. Governments around the world are seeking ways to contain costs through alternative reimbursement models. North America currently dominates the market due to an established healthcare system and higher healthcare expenditures per capita. Europe is also a major market though reimbursement structures vary widely by country.
In Asia Pacific, countries like China and India represent sizable opportunities as these reform their healthcare systems and address the needs of expanding middle classes. Private insurers also plays role in complementing public plans. Technology will also disrupt existing arrangements by enabling faster processing of claims and new payment mechanisms. However, privacy and security concerns may impede digital transformation.
Regulatory uncertainty can hamper the market growth as government policies shape how reimbursement evolves. Provider networks must also adapt to reimbursement changes by controlling costs while maintaining quality of care.
Market Challenges: Lack of healthcare infrastructure and resources
Lack of proper healthcare infrastructure and resources can hamper the global healthcare reimbursement market growth. Many developing nations still struggle with basic healthcare facilities and services for their populations. If primary healthcare needs are not met, it becomes very challenging for reimbursement policies and systems to take hold. For instance, according to WHO, in Africa, only 30% of the population has access to basic healthcare services as of 2022. Most rural regions and underdeveloped areas have few or no hospitals, clinics and community health centers. There is also massive shortage of doctors, nurses and other medical professionals across several African nations as majority of trained staff migrate to developed countries due to poor working conditions and low wages at home. Without fundamental healthcare infrastructure and frontline services, people have very little incentive to invest in insurance policies or opt for reimbursement options. Countries like India, Indonesia, Philippines and Kenya have made progress but healthcare accessibility is still not universal. There are huge disparities between urban and rural populations. According to World Bank Data, over 100 million people get pushed below poverty line every year, thus, paying for healthcare needs out of their own pockets in India and China. This is primarily due to lack of public health coverage and affordability of private medical insurance or company plans for lower income demographics.
Market Opportunities: Emerging applications in homeland security and defense sectors
The emergence of complex disease management programs can offer opportunities for the global healthcare reimbursement market growth. As rates of chronic diseases rises around the world due to increasing life expectancies and lifestyle changes, there is growing need for comprehensive and coordinated care over long periods of time. Disease management programs aim to address this need through multidisciplinary care teams that closely monitor patients, ensure these receive recommended treatments and screenings, and provide education to empower patients in self-managing their conditions. This approach lead to improved health outcomes as compared to routine or episodic care, especially for complex patients with multiple chronic diseases that require inputs from several medical specialists. For example, diabetes management programs that emphasize regular checkups, diet and lifestyle counseling, and coordinating care among primary doctors, endocrinologists and other providers can reduce hospitalizations and healthcare costs for patients with both diabetes and heart disease, according to a 2021 study conducted across nine European countries.
Discover high revenue pocket segments and roadmap to it: Download Free Sample
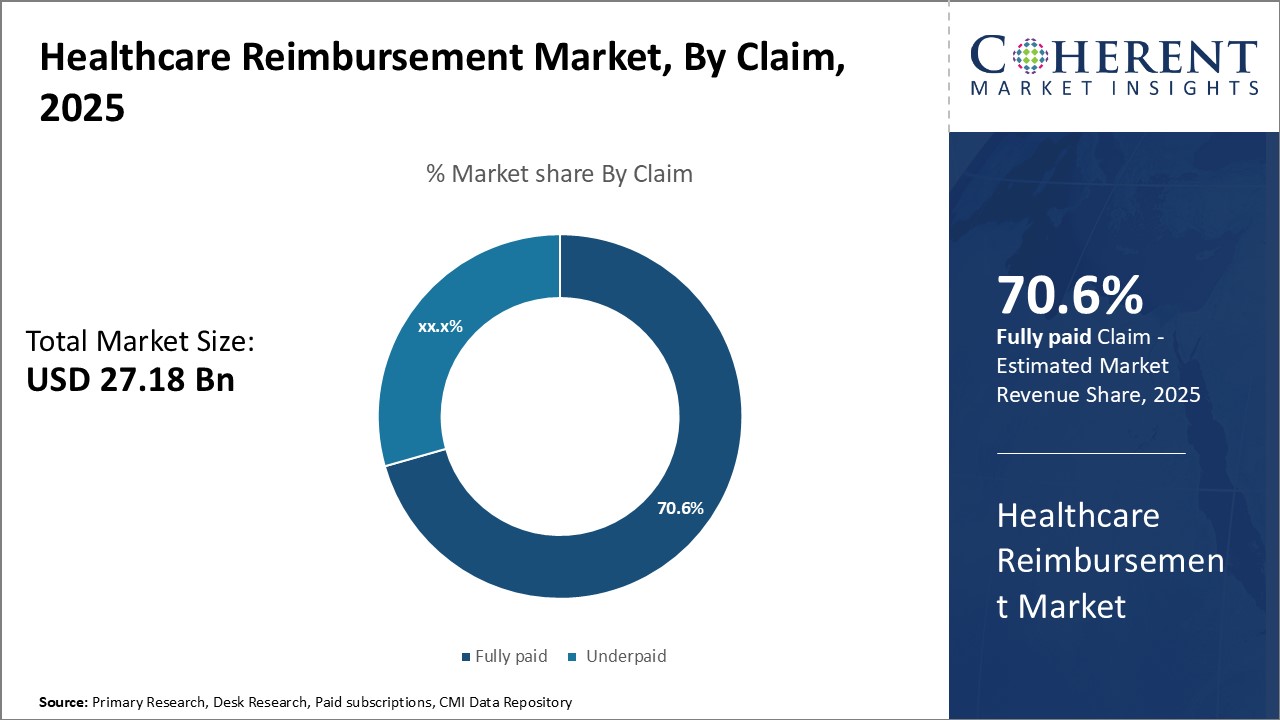
By Claim- Government Support Boosts Fully Paid Segment
In terms of claim, fully paid segment is estimated to contribute the highest market share of 70.6% in 2025, owing to strong government support towards healthcare coverage. Various governments across the globe are promoting universal healthcare through schemes that offer coverage for medical expenses. This encourages more people to opt for comprehensive insurance plans that cover expenses fully without any out-of-pocket payment. The favorable regulations have also spurred competition among insurers to enroll more customers by proposing attractive fully paid options. Employer-sponsored group insurance is a popular mode for providing fully paid healthcare benefits to employees. With growing emphasis on employee wellness, companies find it important to lessen the financial burden through such plans in order to retain skilled workforce.
By Payer- Higher Spending Capacity Boosts Private Payers Segment
In terms of payer, private payers segment is estimated to contribute the highest market share of 60.7% in 2025, owing to their higher spending capacity. Individuals and families with higher disposable incomes prefer spending on private medical insurance or pay directly from pocket. Moreover, many high-income groups seek exclusive care at premium healthcare facilities, which require settling bills privately. Comprehensive private plans offer flexibility in terms of choice of providers and customized coverage. With growing health awareness, people are willing to pay more for quality services and faster access provided by private channels. This boosts preference over public options with limited coverage or long waiting periods.
By Service Provider- Proximity and Flexibility Boosts Physician Office Visits
In terms of service providers, physician office segment is estimated to contribute the highest market share of 35.7% in 2025 as it offers proximity and flexibility. People generally prefer visiting doctors close to their homes for common health issues rather than going to distant hospitals. This saves travel time and effort significantly. Physician clinics also allow quicker appointments and walk-in visits, which is convenient for people. Furthermore, physicians have established relationships with patients over years which encourages repeat visits. Such outpatient services have comparatively lower costs than in-patient treatments. With growing chronic diseases, people are increasingly opting for follow-up consultations and regular check-ups at physician offices.
Regional Insights
Need a Different Region or Segment? Download Free Sample
The United States healthcare reimbursement market currently dominates the global landscape with 38.7% share in 2025 and is primed to retain its pole position in the coming years. As the nation with the highest healthcare spending globally, developments and reforms in the U.S. system have widespread implications for the entire industry. Countries around the world closely watch policy changes and payment models emerging from the country's massive US$ 3.6 trillion annual healthcare expenditures.
While public healthcare programs Medicare and Medicaid remain mainstays, private medical insurance still covers a majority of Americans. However, payers are deploying new strategies like reference pricing and value-based arrangements to stem rising costs from providers. Consolidation among insurance firms has also increased their bargaining power over prices. The U.S. continues refining its complex reimbursement infrastructure which many developing healthcare systems seek to emulate over time.
China is fast emerging as the most promising healthcare reimbursement market globally. Bolstered by Beijing's healthcare reform initiatives and the massive rise of its middle-class segment, the Chinese reimbursement sector has expanded rapidly over the past decade. Both public and private schemes have proliferated to meet the coverage needs of its vast 1.4 billion population. The government is also emphasizing healthcare infrastructure development in rural and suburban segments where reimbursement penetration remains low.
Market Report Scope
Healthcare Reimbursement Market Report Coverage
| Report Coverage | Details | ||
|---|---|---|---|
| Base Year: | 2024 | Market Size in 2025: | USD 27.18 Bn |
| Historical Data for: | 2020 To 2024 | Forecast Period: | 2025 To 2032 |
| Forecast Period 2025 to 2032 CAGR: | 17.6% | 2032 Value Projection: | USD 84.60 Bn |
| Geographies covered: |
|
||
| Segments covered: |
|
||
| Companies covered: |
UnitedHealth Group, Aviva, Allianz, CVS Health Corporation, Bupa, Aon plc, Cigna Corporation, Centene Corporation, Anthem, Inc., Blue Cross Blue Shield Association (BCBSA), Humana Inc., WellCare Health Plans, Inc., Medicaid Services (CMS), Health Care Service Corporation (HCSC), Anthem Blue Cross Blue Shield, Molina Healthcare, Inc., Kaiser Permanente |
||
| Growth Drivers: |
|
||
| Restraints & Challenges: |
|
||
Uncover macros and micros vetted on 75+ parameters: Get instant access to report
Market Segmentation
- Claim Insights (Revenue, USD Bn, 2020 - 2032)
- Fully paid
- Underpaid
- Payer Insights (Revenue, USD Bn, 2020 - 2032)
- Private Payers
- Public Payers
- Service Provider Insights (Revenue, USD Bn, 2020 - 2032)
- Physician office
- Hospitals & Clinics
- Diagnostic Laboratories
- Medical Equipment & Supplies
- Others
- Regional Insights (Revenue, USD Bn, 2020 - 2032)
- North America
- U.S.
- Canada
- Latin America
- Brazil
- Argentina
- Mexico
- Rest of Latin America
- Europe
- Germany
- U.K.
- Spain
- France
- Italy
- Russia
- Rest of Europe
- Asia Pacific
- China
- India
- Japan
- Australia
- South Korea
- ASEAN
- Rest of Asia Pacific
- Middle East
- GCC Countries
- Israel
- Rest of Middle East
- Africa
- South Africa
- North Africa
- Central Africa
- North America
- Key Players Insights
- UnitedHealth Group
- Aviva
- Allianz
- CVS Health Corporation
- Bupa
- Aon plc
- Cigna Corporation
- Centene Corporation
- Anthem, Inc.
- Blue Cross Blue Shield Association (BCBSA)
- Humana Inc.
- WellCare Health Plans, Inc.
- Medicaid Services (CMS)
- Health Care Service Corporation (HCSC)
- Anthem Blue Cross Blue Shield
- Molina Healthcare, Inc.
- Kaiser Permanente
Share
Share
About Author
Manisha Vibhute is a consultant with over 5 years of experience in market research and consulting. With a strong understanding of market dynamics, Manisha assists clients in developing effective market access strategies. She helps medical device companies navigate pricing, reimbursement, and regulatory pathways to ensure successful product launches.
Missing comfort of reading report in your local language? Find your preferred language :
Transform your Strategy with Exclusive Trending Reports :
Frequently Asked Questions
EXISTING CLIENTELE
Joining thousands of companies around the world committed to making the Excellent Business Solutions.
View All Our Clients
