Global Healthcare Payer Services Market Size and Forecast 2025-2032
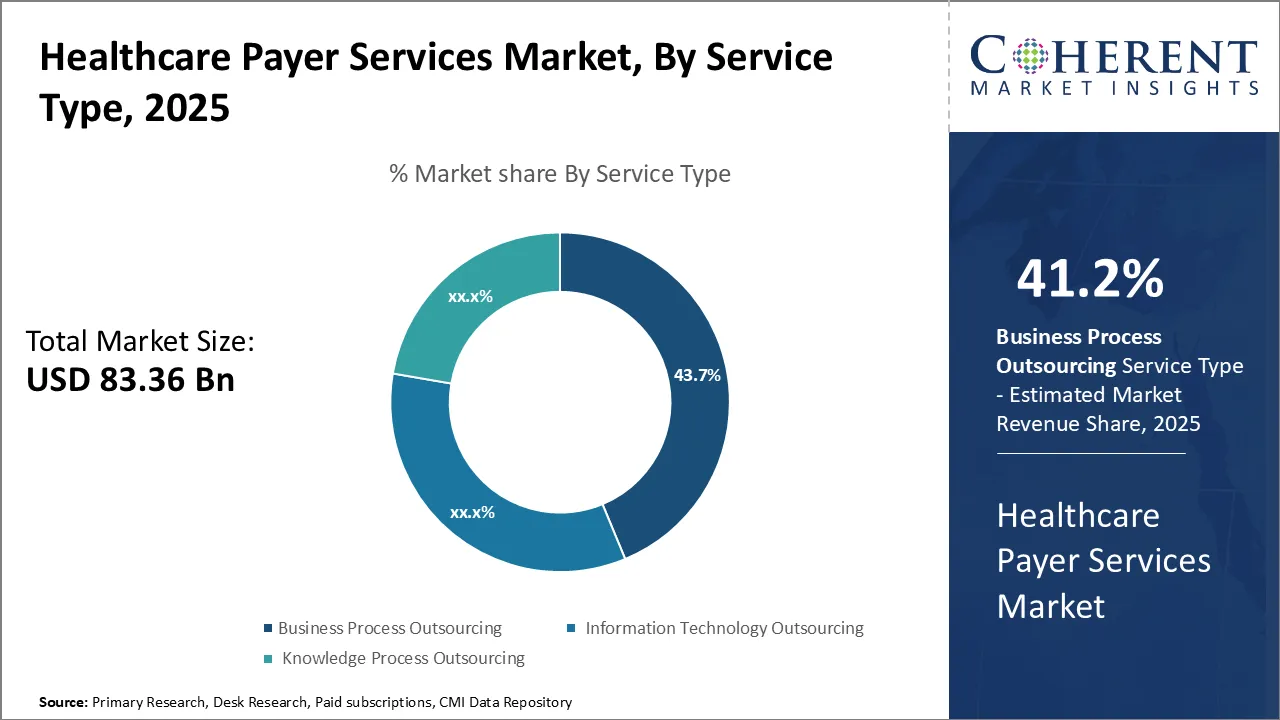
Global healthcare payer services market is estimated to be valued at USD 83.36 Bn in 2025 and is expected to reach USD 158.45 Bn by 2032, exhibiting a compound annual growth rate (CAGR) of 9.6% from 2025 to 2032.
Key Takeaways of the Global Healthcare Payer Services Market
- In terms of service type, the business process outsourcing segment is estimated to contribute the highest market share of 41.2% in 2025.
- In terms of application, the claims management services segment is estimated to contribute the highest market share of 30.62% in 2025.
- In terms of end user, the private payers segment is estimated to contribute the highest market share of 50.1% in 2025.
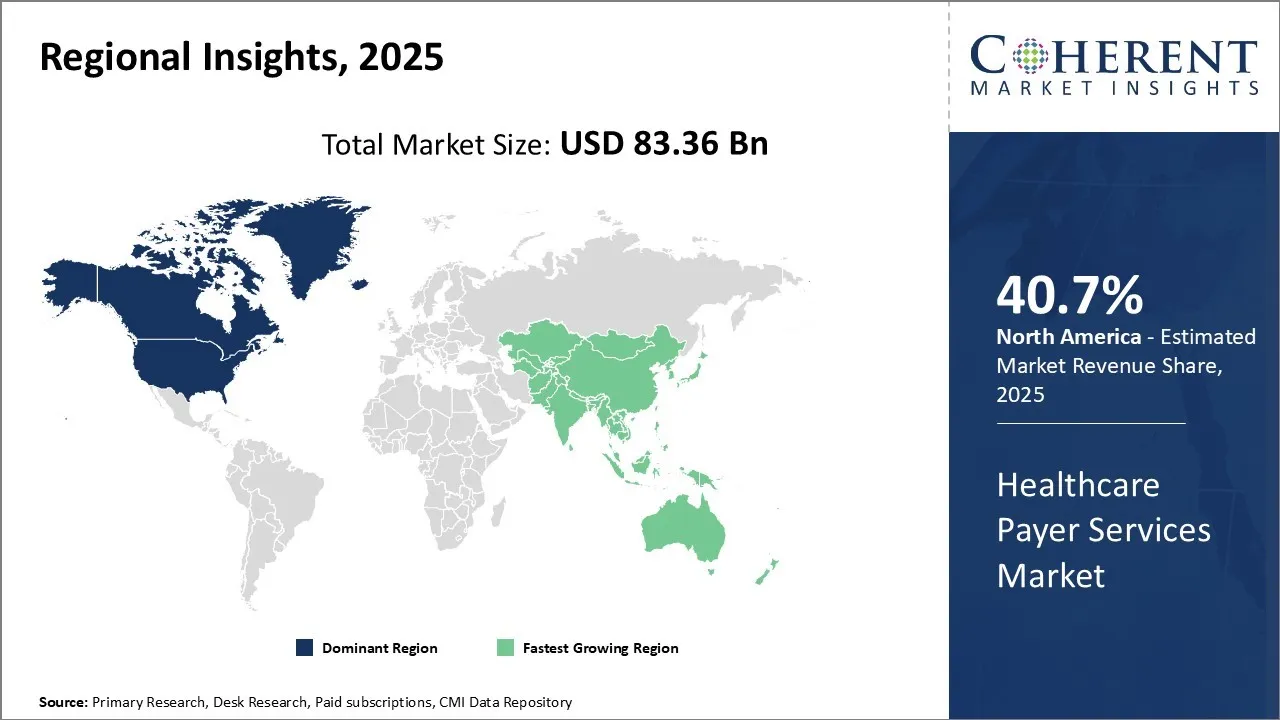
- North America dominates the global healthcare payer services market with an estimated market share of 40.7% in 2025.
Market Overview
Global healthcare payer services market growth is driven by increasing healthcare costs and rising governments' focus on improving the efficiency of payer organizations. There has been growing demand for technologies like artificial intelligence, robotic process automation, Blockchain, and predictive analytics among payer organizations to enhance their offerings and operations. Key market players are focusing on mergers & acquisitions and partnerships to expand their product and service portfolio. For instance, in 2022, UnitedHealth Group acquired Change Healthcare to integrate technology and analytics into clinical and payment processes. Rising chronic diseases due to changing lifestyles also boost the need for efficient healthcare payer services globally.
Impact of AI on the Global Healthcare Payer Services Market
- AI is revolutionizing healthcare operations by automating tasks like prior authorization, which cuts decision times from days to minutes, predicting patient risk, leading to a 15% reduction in hospitalizations, and detecting fraud, decreasing fraudulent payments by 25%.
- AI significantly improves member engagement and outcomes. UnitedHealthcare's AI platform, for instance, offers personalized care, resulting in a 22% drop in preventable hospital readmissions and an 18% boost in medication adherence.
- Strategic AI adoption is crucial for the future of healthcare. It transforms passive data into actionable insights, drives efficiency, enhances member-centricity, and is projected to save the industry USD 17 billion annually by 2027.
Micro and Macro Economic Factors Impacting the Healthcare Payer Services Market
- Healthcare costs are soaring, driven by an aging global population and expensive treatments, prompting governments to push for cost-cutting measures like AI-driven claims processing and value-based care.
- Geopolitical shifts and economic cycles significantly impact healthcare payers, leading to increased focus on regulatory compliance, digital transformation, and resource optimization, as seen with the accelerated adoption of telehealth during the pandemic.
- Technological innovation and consumer demand for personalized care are reshaping the industry, with payers investing in AI and data analytics to streamline operations, reduce costs, and offer customized services like real-time claims tracking and personalized premiums.
- The healthcare payer services market is experiencing significant consolidation, with large acquisitions and partnerships between smaller players and tech firms aiming to enhance operational efficiency and competitive advantage.
Current Events and Its Impact
|
Current Events |
Description and its impact |
|
U.S. Healthcare Policy Shifts (Macro-Level)
|
|
|
EU Regulatory Overhaul (Regional)
|
|
Uncover macros and micros vetted on 75+ parameters: Get instant access to report
To learn more about this report, Download Free Sample
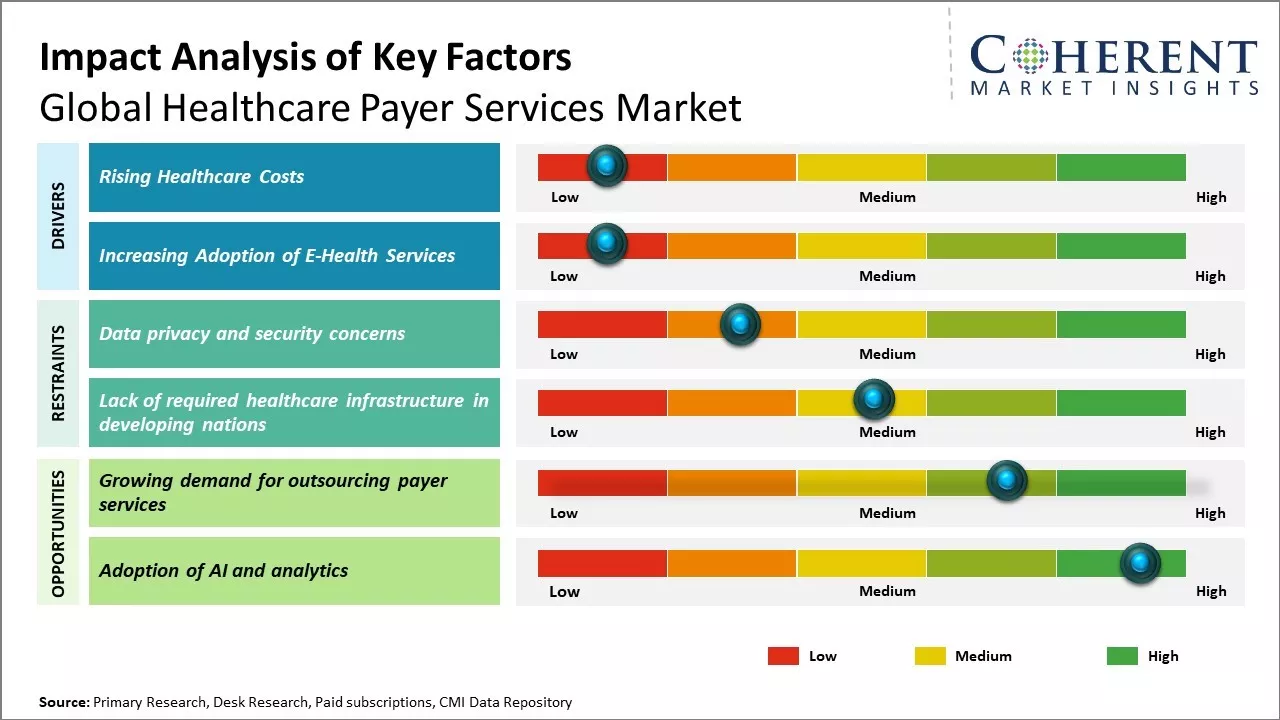
Rising Healthcare Costs
Rising healthcare costs can drive the market growth. Healthcare expenditure has been increasing at a rate higher than the economic growth and rate of inflation in many countries. This unsustainable rise in healthcare costs is driven by factors like increasing demand for quality healthcare services due to a growing aging population, a rise in lifestyle diseases, new and expensive medical technologies, drugs, and treatments. This has significantly boosted the demand for professional healthcare payer services. Healthcare payers help individuals and organizations tackle rising medical costs in a planned manner through tools like health insurance plans, membership packages, claims processing, utilization management, care coordination, and others.
For instance, in the U.S., total healthcare spending reached an estimated USD 4.9 trillion in 2023, representing 17.6% of the nation's GDP. This substantial expenditure highlights the critical need for sophisticated healthcare payer services to navigate complex insurance claims and optimize financial flows within the healthcare system.
Increasing Adoption of E-Health Services
The rising adoption of e-health services, including telemedicine, is a key driver for the healthcare payer services market. Digital access to care allows patients to consult doctors, order refills, and view records remotely, enhancing accessibility, especially for those in remote areas. This shift, accelerated by the pandemic, has led payers to innovate, developing new solutions for claims and customer experience using data analytics. For instance, in April 2024, eHealth Inc. launched its "eHealth Perks" rewards program, enrolling over 200,000 Medicare customers, demonstrating the industry's commitment to integrating digital convenience and virtual care into payer offerings.
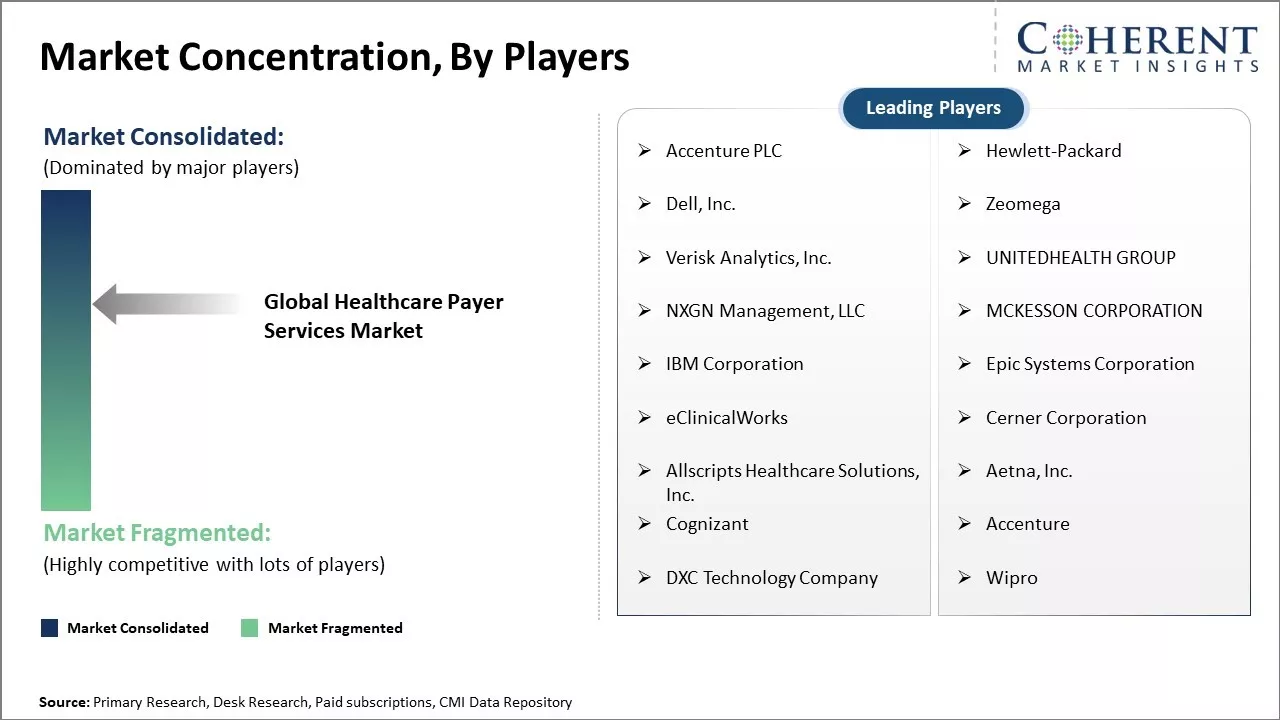
Market Concentration and Competitive Landscape
To learn more about this report, Download Free Sample
Analyst View
- The global healthcare payer services market is primarily expanding due to rising healthcare costs, the increasing need for cost reduction within the industry, and the imperative for payers to enhance efficiencies and optimize processes.
- Data privacy and security concerns present a significant challenge to market growth. As payers manage larger volumes of sensitive data and outsource more services, ensuring robust confidentiality and security of patient information is crucial for maintaining industry trust.
- The Asia Pacific region is poised to offer lucrative opportunities and is expected to lead market growth. This is driven by increasing medical expenditures, rising healthcare insurance penetration, and the growing demand for improved healthcare infrastructure in its developing nations.
- Both North America and Europe will also display notable growth. North America's expansion is fueled by ongoing healthcare reforms and the adoption of advanced technologies, while Europe's growth stems from government mandates to modernize systems and control costs, boosting reliance on outsourcing.
Market Opportunity: Growing Demand for Outsourcing Payer Services
There is a growing demand for outsourcing payer services that can offer opportunities for the global healthcare payer services market growth. As the cost of healthcare increases around the world, payers are under pressure to enhance efficiencies, reduce costs, and provide a better customer experience. This compelled many payers to outsource non-core operations like claims processing, customer service support, enrollment services, benefit management, and others to third-party service providers.
Outsourcing allows payers to focus on their core competencies while leveraging the expertise, economies of scale, and automation capabilities of outsourcing companies. The outsourced payer services help improve processing turnaround time, claims accuracy, and enhance customer and provider satisfaction through personalized services. For instance, advanced technologies like AI, analytics, cloud, and robotics are being adopted by outsourcing companies to streamline workflows and drive higher productivity.
Global Healthcare Payer Services Market Insights, By Service Type
In terms of service type, the business process outsourcing segment is estimated to contribute the highest market share of 41.2% in 2025, owing to payers' focus on optimizing costs through the outsourcing of non-core functions. Business process outsourcing allows players to focus internal resources on member acquisition and retention, product development, and care management. Outsourcing various back-office functions such as claims processing, enrollment services, premium billing, and payment processing to external specialized providers enables payers to reduce expenditures on physical infrastructure, IT systems, and training/managing large internal workforces for administrative tasks.
Specialized BPO providers are able to achieve economies of scale through standardized centralized platforms and processes that service multiple payer clients simultaneously. BPO vendors continually invest in automation, robotics, and artificial intelligence to make processes more efficient. Payers can leverage such continuous improvements by their outsourcing partners without having to modernize existing legacy internal systems.
Global Healthcare Payer Services Market Insights, By Application
In terms of application, the claims management services segment is estimated to contribute the highest market share of 30.62% in 2025, due to growing healthcare membership as well as increasing complexity of claims. As healthcare coverage expands to include more beneficiaries, the overall volume as well as the complexity of medical claims filed is rising rapidly. Meanwhile, newer specialized therapy areas, procedures involving novel medical technologies, and inconsistencies across provider billing practices have made the process of reviewing, approving, and reimbursing claims more challenging.
Expert third party claims administrators also apply AI-enabled robust auditing and fraud detection tools to review claims for inconsistencies, duplicates, and potential fraudulent activities. Their analytics capabilities and access to massive inter-client claims data help identify risk patterns and root causes more effectively.
Global Healthcare Payer Services Market Insights, By End User
In terms of end user, the private payers segment is estimated to contribute the highest market share of 50.1 % in 2025, driven by their need to contain expenditures. Private insurers face rising cost pressures due to increasing healthcare inflation, growing consumer demand for richer benefits, and the need to remain competitive on premiums. Outsourcing non-clinical functions is an effective strategy to extract savings without compromising on services or payment accuracy. Private payers are able to transfer sizeable back-office operational costs to experienced service vendors by outsourcing entire business functions or selective processes.
Vendors achieve scale benefits through standardized, centralized platforms and delivery models shared among multiple clients. This creates a noticeable cost differential as compared to private payers maintaining these capabilities in-house. It allows them to pass on savings to employers and consumers in the form of lower premiums or richer plan designs to boost their market share.
Regional Insights
To learn more about this report, Download Free Sample
North America Healthcare Payer Services Industry Trends and Market Analysis
North America dominates the global healthcare payer services market with an estimated market share of 40.7% in 2025. The U.S. accounts for the lion's share of the market due to the presence of several leading healthcare insurance companies and managed care organizations. The large size of the U.S. private healthcare system has led to the emergence of many third-party administrators and benefit managers who work closely with insurance firms to manage claims, process billing, and implement various government-sponsored programmes. Moreover, medical coding and billing services have proliferated in the U.S. due to the need for paperwork reduction and maintaining compliance with regulatory standards. Many U.S. healthcare payers also outsource non-core services like customer support and back-office operations to specialist BPO vendors.
For instance, the North America healthcare payer services market size surpassed USD 54.54 billion in 2024 and is expected to grow at a CAGR of 7.09% during the forecast period. Private payers hold a significant share, with over 63% of the market, driven by demand for advanced solutions to improve member engagement and claims processing. The region also saw 65% of global healthcare private equity deal value in 2024, indicating strong investment in the sector.
Asia Pacific Healthcare Payer Services Industry Trends and Market Analysis
Asia Pacific is expected to emerge as the fastest growing region, led by China and India. In China, the government is focusing heavily on expanding basic medical insurance to a wider population, which has boosted the third- party administration sector. Meanwhile, several global insurance giants have either set up subsidiaries or partnered with local insurers to gain a foothold in China's promising healthcare market. In India, increasing expenditure on healthcare and medical tourism are encouraging private insurance providers as well public insurers to strengthen their managed care capabilities and rely more on payers services. Low costs have attracted many global companies to establish offshore delivery centers for payer functions like claims processing and customer support in countries like India.
For instance, the Asia Pacific healthcare payer services market is projected to reach an estimated USD 13.02 billion by 2030, exhibiting a CAGR of 7.7% during the forecast period. China's basic medical insurance covered over 95% of its population as of late 2024, while India's healthcare expenditure reached INR 6.1 lakh crore in 2024-25. India also attracted an estimated 7.3 million medical tourists in 2024, becoming the largest private equity healthcare investment destination in APAC, with 26% of deal volume.
India Healthcare Payer Services Industry Trends and Market Analysis
The India healthcare payer services industry is witnessing robust growth, driven by rising healthcare costs, increasing health insurance penetration, and the government's strong push for digital health transformation, exemplified by initiatives like the Ayushman Bharat Digital Mission. This digitalization, significantly accelerated by the pandemic, is leading to increased adoption of telemedicine and digital health records, streamlining claims processing and enhancing patient experience. While challenges related to data privacy and cybersecurity persist, the growing awareness about health insurance benefits and strategic investments in health tech are creating a dynamic and opportunity-rich market for payers.
U.S. Healthcare Payer Services Industry Trends and Market Analysis
The U.S. healthcare payer services market is undergoing significant transformation, driven by escalating healthcare costs, complex regulatory changes, and a strong push towards digital innovation. Payers are increasingly investing in advanced technologies like AI and machine learning to streamline claims processing, combat fraud, and enhance member engagement. The shift towards value-based care models also compels payers to focus on data analytics for improved patient outcomes and cost management. While concerns around data privacy and security remain, the overall trend points to a digitally mature, efficient, and patient-centric future for U.S. healthcare payers.
Market Report Scope
Healthcare Payer Services Market Report Coverage
| Report Coverage | Details | ||
|---|---|---|---|
| Base Year: | 2024 | Market Size in 2025: | USD 83.36 Bn |
| Historical Data for: | 2020 To 2024 | Forecast Period: | 2025 To 2032 |
| Forecast Period 2025 to 2032 CAGR: | 9.6% | 2032 Value Projection: | USD 158.45 Bn |
| Geographies covered: |
|
||
| Segments covered: |
|
||
| Companies covered: |
Accenture PLC, Institute BCN Esthetics S.L., Hewlett-Packard, Dell, Inc., Zeomega, Verisk Analytics, Inc., UNITEDHEALTH GROUP, NXGN Management, LLC, MCKESSON CORPORATION, IBM Corporation, Epic Systems Corporation, eClinicalWorks, Cerner Corporation, Allscripts Healthcare Solutions, Inc., Aetna, Inc., Cognizant, Accenture, DXC Technology Company, and Wipro |
||
| Growth Drivers: |
|
||
| Restraints & Challenges: |
|
||
Uncover macros and micros vetted on 75+ parameters: Get instant access to report
Global Healthcare Payer Services Market Industry News
- In 2025, Optum, a subsidiary of UnitedHealth Group and a major provider of healthcare services, has continued to roll out expanded AI-powered solutions aimed at optimizing various aspects of payer operations.
- Elevance Health (formerly Anthem) announced an expanded partnership with Innovaccer in early 2025, a leading healthcare data platform. This collaboration aims to enhance data interoperability and analytics capabilities for Elevance Health's payer services, enabling more personalized member engagement and improved population health management across their various health plans.
- In June 2024, Cognizant announced the acquisition of Belcan, a significant move that strengthens its capabilities in digital engineering, research and development (R&D) services.
- In 2025, Centene Corporation, a prominent multi-national healthcare enterprise, announced a collaboration with Health Gorilla to facilitate secure and efficient healthcare data exchange.
Market Segmentation
- By Service Type
- Business Process Outsourcing
- Information Technology Outsourcing
- Knowledge Process Outsourcing
- By Application
- Claims Management Services
- Integrated Front Office Service and Back Office Operations
- Member Management Services
- Provider Management Services
- Billing and Accounts Management Services
- Analytics and Fraud Management Services
- HR Services
- Payment Management Services
- Audit and Analysis Systems
- By End User
- Private Payers
- Public Payers
- By Region
- North America
- U.S.
- Canada
- Latin America
- Brazil
- Argentina
- Mexico
- Rest of Latin America
- Europe
- Germany
- U.K.
- Spain
- France
- Italy
- Russia
- Rest of Europe
- Asia Pacific
- China
- India
- Japan
- Australia
- South Korea
- ASEAN
- Rest of Asia Pacific
- Middle East
- GCC Countries
- Israel
- Rest of Middle East
- Africa
- South Africa
- North Africa
- Central Africa
- North America
- Company Profiles
- Accenture PLC
- Institute BCN Esthetics S.L.
- Hewlett-Packard
- Dell, Inc.
- Zeomega
- Verisk Analytics, Inc.
- UNITEDHEALTH GROUP
- NXGN Management, LLC
- MCKESSON CORPORATION
- IBM Corporation
- Epic Systems Corporation
- eClinicalWorks
- Cerner Corporation
- Allscripts Healthcare Solutions, Inc.
- Aetna, Inc.
- Cognizant
- Accenture
- DXC Technology Company
- Wipro
Sources
Stakeholders
- Healthcare Service Providers
- Healthcare Insurance Providers
- Technology Platform Providers
- Industry Consultants and Experts
- Others
Databases
- World Bank Database
- OECD Healthcare Database
- International Monetary Fund (IMF)
- Others
Magazines
- Healthcare IT News
- Managed Healthcare Executive
- Healthcare Finance Magazine
- Others
Journals
- Journal of Healthcare Management
- Journal of Health Economics
- American Journal of Managed Care
- Others
Newspapers
- The Wall Street Journal
- Financial Times
- The Economic Times
- Others
Associations
- American Health Information Management Association (AHIMA)
- Healthcare Financial Management Association (HFMA)
- America's Health Insurance Plans (AHIP)
- Others
Public Domain Sources
- World Health Organization (WHO)
- Centers for Medicare & Medicaid Services (CMS)
- U.S. Department of Health and Human Services (HHS)
- Others
Proprietary Elements
- CMI Data Analytics Tool, Proprietary CMI Existing Repository of information for last 8 years
Share
Share
About Author
Komal Dighe is a Management Consultant with over 8 years of experience in market research and consulting. She excels in managing and delivering high-quality insights and solutions in Health-tech Consulting reports. Her expertise encompasses conducting both primary and secondary research, effectively addressing client requirements, and excelling in market estimation and forecast. Her comprehensive approach ensures that clients receive thorough and accurate analyses, enabling them to make informed decisions and capitalize on market opportunities.
Missing comfort of reading report in your local language? Find your preferred language :
Transform your Strategy with Exclusive Trending Reports :
Frequently Asked Questions
EXISTING CLIENTELE
Joining thousands of companies around the world committed to making the Excellent Business Solutions.
View All Our Clients